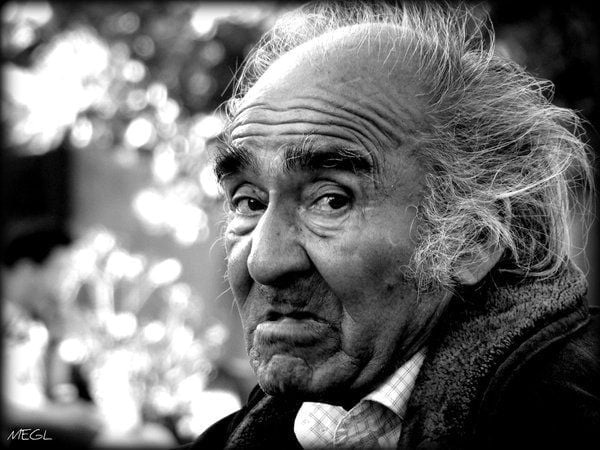
Δεν αποτελεί φυσιολογική επίπτωση της γήρανσης
Η κατάθλιψη στην τρίτη ηλικία είναι μια πραγματική αλλά θεραπεύσιμη παθολογική κατάσταση, όπως ο διαβήτης και η υπέρταση. Δεν αποτελεί φυσιολογική επίπτωση της γήρανσης, μολονότι οι ηλικιωμένοι έχουν αυξημένο κίνδυνο για την εμφάνισή της.
Πρόκειται για μια διαταραχή της διάθεσης, στην οποία συναισθήματα θλίψης, απώλειας, θυμού ή απογοήτευσης διαχέονται στην καθημερινότητα και επιδρούν για εβδομάδες ή και περισσότερο, επηρεάζοντας την ποιότητα της ζωής αλλά και τη λειτουργικότητα του ανθρώπου. Δεν πρόκειται για “ακεφιές”, ή για το πένθος πχ. από το θάνατο ενός αγαπημένου. Τις περισσότερες φορές, δεν πρόκειται καν για τη μείζονα κατάθλιψη που μας απασχολεί στους ενήλικες (με επίπτωση 1-5% στους ηλικιωμένους), αλλά για υποσυνδρομική κατάθλιψη που βασανίζει 15% όλων των περιπατητικών ηλικιωμένων και πολύ μεγαλύτερο ποσοστό εκείνων που χρειάζονται φροντίδα στο σπίτι, ή νοσοκομειακή περίθαλψη για οποιοδήποτε λόγο.
Κι όμως, μόλις 10% αυτών των ανθρώπων λαμβάνει θεραπεία.
Στους ηλικιωμένους η κατάθλιψη εμφανίζεται συχνά μαζί με άλλες παθήσεις και αναπηρίες και διαρκεί περισσότερο. Συγκεκριμένα, γνωρίζουμε ότι περίπου 80% των ηλικιωμένων έχουν τουλάχιστον μία χρόνια πάθηση, ενώ 50% πάσχουν από δύο ή περισσότερες. Η κατάθλιψη στην τρίτη ηλικία επηρεάζει αρνητικά τις συνυπάρχουσες παθήσεις. Για παράδειγμα, διπλασιάζει τον κίνδυνο καρδιακών παθήσεων και αυξάνει τον κίνδυνο θανάτου από αυτές. Επίσης, αυξάνει τον κίνδυνο αυτοκτονίας έως και δύο φορές σε σχέση με τον γενικό πληθυσμό (ηλικίες 80-84), με τους διαζευγμένους ή χήρους άνδρες να διατρέχουν τον υψηλότερο κίνδυνο.
Για όλους τους παραπάνω λόγους, έχουμε την υποχρέωση να διασφαλίζουμε ότι ένας ηλικιωμένος άνθρωπος με σημεία και συμπτώματα της νόσου αξιολογείται και θεραπεύεται, ακόμη και αν αυτά είναι ήπια. Οι δε οικογένειες οφείλουν να ανησυχούν για τους ηλικιωμένους συγγενείς που πάσχουν από κατάθλιψη και διαβιούν μόνοι.
Ένας γονέας που δεν τρώει για περισσότερες από μερικές ημέρες, ή χάνει το ενδιαφέρον σε δραστηριότητες που προηγούμενα έμοιαζαν ευχάριστες για περισσότερο από δύο εβδομάδες, θα μπορούσε να πάσχει με κατάθλιψη. Είναι πολύ συνηθισμένο οι ηλικιωμένοι συγγενείς μας να μας απαντούν ότι «δεν αισθάνονται λυπημένοι» ή ότι «δεν νιώθουν μόνοι», μόνο και μόνο επειδή δεν επιθυμούν να γίνονται βάρος στην υπόλοιπη οικογένεια. Αντ’ αυτού, παρουσιάζουν σημάδια αγωνίας, πχ. στύβοντας τα χέρια τους, είναι ταραγμένοι ή ευερέθιστοι χωρίς αιτία, ή ακόμη και υπερκινητικοί.
Σε κάθε περίπτωση, πρέπει να υποψιαζόμαστε την κατάθλιψη όταν ένας ηλικιωμένος αναφέρει ή εμφανίζει:
• Συναισθήματα απόγνωσης ή και απαισιοδοξίας
• Αισθήματα ενοχής, αναξιότητας ή και ανικανότητας
• Ευερεθιστότητα, ανησυχία
• Απώλεια ενδιαφέροντος για δραστηριότητες ή χόμπι που προηγούμενα πρόσφεραν ευχαρίστηση
• Κόπωση και μειωμένη ενέργεια
• Συναισθηματική απάθεια
• Δυσκολία συγκέντρωσης, δυσκολία στην ανάκληση λεπτομερειών και στη λήψη αποφάσεων
• Αϋπνία, πρόωρη αφύπνιση, ή υπερβολικό ύπνο
• Υπερκατανάλωση τροφής, ή απώλεια όρεξης
• Σκέψεις αυτοκτονίας ή απόπειρες αυτοκτονίας
• Επίμονα άλγη ή πόνους, όπως πονοκέφαλοι, κράμπες, ή πεπτικά ενοχλήματα που δεν παρέρχονται ακόμη και με θεραπείες που απευθύνονται σε αυτά
Μάλιστα η παρουσία των σωματικών επακόλουθων της κατάθλιψης, όπως η σοβαρή αυχεναλγία και η επίμονη οσφυαλγία είναι προειδοποιητικά συμπτώματα που υποεκτιμούνται κατά κανόνα.
Η προχωρημένη ηλικία συχνά συνοδεύεται από την απώλεια όλων των συστημάτων κοινωνικής στήριξης, για παράδειγμα με τον θάνατο ενός συζύγου, ή των αδελφών, τη συνταξιοδότηση, τη μετεγκατάσταση της κατοικίας, κ.α. Εξαιτίας τέτοιων μεταβολών στις συνθήκες ζωής αλλά και της αντικειμενικής λειτουργικής επιβράδυνσης που αντιμετωπίζει ένας άνθρωπος από τη βιολογική φθορά του χρόνου, τόσο η οικογένεια όσο και οι ιατροί ενίοτε προσπερνούν τα σημάδια της κατάθλιψης, με συνέπεια να καθυστερεί σημαντικά η αποτελεσματική αντιμετώπιση. Για αυτό, πολλοί ηλικιωμένοι άνθρωποι καταδικάζονται να παλεύουν με βασανιστικά συναισθήματα χωρίς λόγο.
Στην κατάθλιψη συμβάλλουν πάντοτε πολλοί παράγοντες, όπως τα χαμηλά επίπεδα των βασικών χημικών νευροδιαβιβαστών στον εγκέφαλο (σεροτονίνη, νορεπινεφρίνη), το οικογενειακό ιστορικό κατάθλιψης και ασφαλώς τα τραυματικά γεγονότα της ζωής. Επιπρόσθετα, συμβάλλουν επιπλοκές που σχετίζονται με τη γήρανση όπως:
• Η περιορισμένη κινητικότητα και η κατάργηση της ανεξαρτησίας που αυτή συνεπάγεται
• Η απομόνωση
• Οι σκέψεις για το επικείμενο τέλος της ζωής
• Η μετάβαση από την εργασία στη συνταξιοδότηση
• Οι οικονομικές δυσκολίες
• Η παρατεταμένη κατάχρηση ουσιών
• Οι θάνατοι φίλων και αγαπημένων
• Η απομάκρυνση ή και αποξένωση των παιδιών
• Η χηρεία ή το διαζύγιο
• Οι χρόνιες παθήσεις
Δυστυχώς, το στίγμα που συνδέεται με την ψυχική ασθένεια και την ψυχιατρική θεραπεία είναι πιο ισχυρό μεταξύ των ηλικιωμένων σε σχέση με τους νεότερους. Το στίγμα μπορεί να αποτρέψει τους ηλικιωμένους από την αναγνώριση του προβλήματος και να απομακρύνει από την παραδοχή του. Ακόμη περισσότερο, συμβαίνει συνήθως οι ηλικιωμένοι άνθρωποι και οι οικογένειές τους να αποδίδουν τα συμπτώματα της κατάθλιψης σε «κανονικές» αντιδράσεις στο στρες της ζωής, στις ματαιώσεις, ή στο γήρας.
Επειδή το αίσθημα κόπωσης, η απώλεια όρεξης και οι δυσκολίες στον ύπνο αποτελούν κοινά συμπτώματα με τη διαδικασία της γήρανσης, ή τις σωματικές ασθένειες, είναι εύκολο να αγνοηθεί μια αρχόμενη κατάθλιψη ή να παρεξηγηθεί με τη γήρανση.
Ειδικά η αϋπνία επισημαίνεται ως ένας ξεχωριστός παράγοντας κινδύνου τόσο για την εμφάνιση της κατάθλιψης στους ηλικιωμένους όσο και για τις υποτροπές της.
Ορισμένες φορές η κατάθλιψη στους ηλικιωμένους εκφράζεται μέσα από σωματικές ενοχλήσεις και όχι με τα τυπικά συμπτώματά της. Και αυτό το φαινόμενο καθυστερεί, με τη σειρά του, την κατάλληλη θεραπεία. Επιπλέον, οι καταθλιπτικοί άνθρωποι μεγαλύτερης ηλικίας δεν αναφέρονται στην κατάθλιψή τους ακόμη και όταν αποδέχονται ότι υποφέρουν με το πρόβλημα, επειδή πιστεύουν ότι δεν υπάρχει καμία ελπίδα για βοήθεια.
Παρόλα αυτά, η διαχείριση της κατάθλιψης προϋποθέτει τη συνεργασία με τον ειδικό. Στην πορεία της διάγνωσης, ο ειδικός θα αποκλείσει την πιθανότητα της συμμετοχής οργανικών διαταραχών που μπορεί να μιμούνται τα συμπτώματα της κατάθλιψης, όπως η αναιμία, η έλλειψη Β12 και φυλλικού οξέος, ο υποθυρεοειδισμός, κ.α. Ακόμη, θα εξετάσει τυχόν υποκείμενες ασθένειες που δυνητικά σχετίζονται και επιπλέκονται με κατάθλιψη, όπως οι διαταραχές στη λειτουργία του θυρεοειδούς, η νόσος Πάρκινσον, οι καρδιαγγειακές παθήσεις, ο καρκίνος, οι άνοιες (όπως η νόσος Alzheimer) και τα αγγειακά εγκεφαλικά επεισόδια.
Σε ό,τι αφορά στο τελευταίο, διαπιστώνουμε ενίοτε ότι οι άνθρωποι που αναπτύσσουν κατάθλιψη για πρώτη φορά σε μεγάλη ηλικία, παρουσιάζουν σημεία ισχαιμικής εγκεφαλοπάθειας από την ανεπαρκή ροή αίματος στους εγκεφαλικούς ιστούς στο έδαφος χρόνιας αρτηριακής υπέρτασης.
Για την καλύτερη διαχείριση της κατάθλιψης στο σπίτι, οι ηλικιωμένοι συνάνθρωποί μας θα πρέπει:
• Να ασκούνται τακτικά, εφόσον συναινεί ο θεράπων
• Να περιβάλλονται με φροντίδα, θετικούς ανθρώπους και διασκεδαστικές δραστηριότητες
• Να έχουν καλές συνήθειες ύπνου
• Να ενημερώνονται ώστε να αναγνωρίζουν τα πρώτα σημάδια της κατάθλιψης και να αναζητούν εξειδικευμένη βοήθεια
• Να αποφεύγουν το αλκοόλ και τις ναρκωτικές ουσίες, συμπεριλαμβανομένων των ηρεμιστικών φαρμάκων χωρίς απόλυτη ένδειξη
• Να λεκτικοποιούν τα συναισθήματά τους και να επικοινωνούν με άλλους ανθρώπους που εμπιστεύονται
• Να λαμβάνουν σωστά τα φάρμακά τους και να συζητούν τις τυχόν παρενέργειες με τον θεράποντα
να περνάμε χρόνο με τους ηλικιωμένους συγγενείς μας
Τα δυσάρεστα γεγονότα της ζωής, συμπεριλαμβανομένου του θανάτου οικείων ή αγαπημένων, της φτώχειας και της απομόνωσης, ενδέχεται να επηρεάζουν τα κίνητρα του ανθρώπου να συνεχίζει τη θεραπεία του. Οι ηλικιωμένοι μπορούν, επίσης, να είναι απρόθυμοι να λαμβάνουν τη θεραπεία τους λόγω παρενεργειών ή του κόστους.
Δεδομένου ότι οι ηλικιωμένοι είναι πιο ευαίσθητοι στα φάρμακα, οι ιατροί οφείλουν να συνταγογραφούν μικρότερες δόσεις σε σχέση με τους ενήλικες. Παρά το γεγονός ότι οι συνυπάρχουσες ασθένειες ενδέχεται να επηρεάζουν την αποτελεσματικότητα των αντικαταθλιπτικών θεραπειών, αυτή η δόκιμη πρακτική απαλλάσσει από το μεγαλύτερο μέρος των παρενεργειών, μολονότι διαπιστώνω ότι δεν εφαρμόζεται με συνέπεια… Η δε ψυχοθεραπεία, που μπορεί να είναι ιδιαίτερα ευεργετική για όσους έχουν υποστεί σημαντικά ψυχοπιεστικά γεγονότα στη διάρκεια της ζωής, δεν προσφέρεται – ή δεν μοιάζει προσβάσιμη – στους ηλικιωμένους της χώρας μας.
Θα ήθελα να μου επιτρέψετε να υπογραμμίσω ότι είναι πολύ σημαντικό να περνάμε χρόνο με τους ηλικιωμένους συγγενείς μας. Να τους ακούμε και να τιμούμε τα συναισθήματά τους. Ο ποιοτικός χρόνος που τους αφιερώνουμε, επιφέρει άμεση ανακούφιση και είναι πραγματική υποστήριξη. Τέλος, αξίζει να σημειώσω ότι έχει σημασία να μην υποκαθιστούμε τους ηλικιωμένους ανθρώπους στις δραστηριότητές τους με σκοπό να τους διευκολύνουμε, επειδή αυτό δυνητικά ενισχύει την αντίληψή τους ότι δεν είναι πλέον χρήσιμοι και ικανοί. Τουναντίον, είναι περισσότερο σκόπιμο να τους βοηθούμε να επιμερίζουν τις δραστηριότητές τους σε περισσότερα και πιο διακριτά βήματα, που εκτελούνται με μεγαλύτερη ευελιξία, και να τους επαινούμε για την προσπάθειά τους.